Bell’s palsy is a form of facial paralysis thought to occur after viral infection. Symptoms such as drooping face, difficulty in closing the eyes on the affected side, drooling, and loss of taste may appear suddenly. Symptoms usually go away on their own within a few weeks, but may be permanent. A physical therapist is trained to assess your condition and provide a treatment plan tailored to Bell’s palsy.
In this article, we’ll look at the symptoms, causes, and treatment of Bell’s palsy. We describe some of the stretching and strengthening techniques we use on some of our clients to help them regain the healthy movement patterns needed for expression and function.
What is Bell’s Palsy?
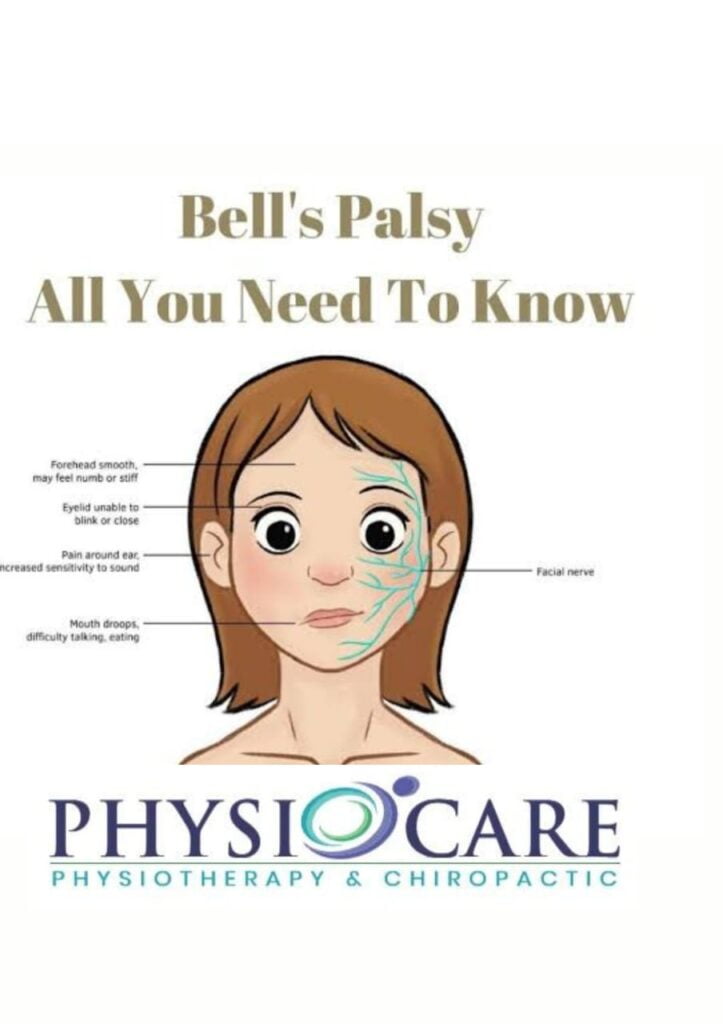
Bell’s palsy, also known as idiopathic facial nerve palsy, is a form of temporary facial paralysis or weakness .It usually affects only one side of the face. However, in rare cases both sides can be affected. Bell’s palsy is thought to be the result of swelling and inflammation of the nerves that control the muscles on one side of the face and can occur after a viral infection. This facial nerve (cranial nerve 7/12)controls the muscles on one side of the face, such as the muscles that control facial expressions such as opening and closing the eye sand smiling. The facial nerve also carries nerve impulses to the lacrimal and salivary glands and to the muscles of the small bones in the center of the ear. It also transmits the sense of taste from the tongue.
In most cases, Bell’s palsy is temporary. Symptoms appear suddenly over 48 to 72 hours and usually improve after a few weeks with or without treatment. Recovery of some or all facial function usually occurs within 6 months. Rarely, Bell’s palsy may recur after the initial symptom shave resolved.
Bell’s palsy is the most common cause of facial paralysis. About 40,000 people are affected in the United States each year. Anyone can be affected, regardless of age or gender, but incidence appears to be highest in the 15-45yearold group.
Bell’s palsy occurs more often in people who:
Are pregnant, especially during the third trimester, or who are in the first week after giving birth
Have preeclampsia
Have an upper respiratory infection, such as the flu or a cold
Have diabetes
Obesity
Hypertension
Upper respiratory ailments
Recurrent attacks of Bell’s palsy are rare. But in some of these cases, there’s a family history of recurrent attacks — suggesting a possible genetic predisposition to Bell’s palsy.
Symptoms of Bell’s Palsy
Because the facial nerve has so many functions and is so complex, damage to the nerve can lead to a range of problems. Symptoms of Bell’s palsy can vary from person to person and range in severity from mild weakness to total paralysis of the facial muscles.
Signs and symptoms of Bell’s palsy appear suddenly and may include:
Rapid onset of mild weakness to total paralysis on one side of your face — occurring within hours to days
Facial droop and difficulty making facial expressions, such as closing your eye or smiling
Asymmetrical smile
Difficult closing the eye on the affected side causing dryness of the eye
Drooling
Pain around the jaw or in or behind your ear on the affected side
Increased sensitivity to sound on the affected side
Headache
A loss of taste
Changes in the quantity of tears and saliva you produce.
What Causes Bell’s Palsy?
The cause of Bell’s palsy is unknown. Swelling and inflammation of the 7th cranial nerve is seen in people with Bell’s palsy. It is believed that reactivation of pre-existing (dormant) viral infections can cause damage. A weakened immune system due to stress, lack of sleep, physical trauma, mild illness, or an autoimmune syndrome has been suggested as the most likely trigger. When the facial nerve becomes swollen and inflamed in response to infection, it puts pressure on the fallopian tubes( the bone tubes through which the nerve travels to the side of the face), limiting blood and oxygen to the nerve cells. Recovery is rapid, and only the myelin sheath (the fatty covering that serves to insulate nerve fibers)is damaged.
How is Bell’s Palsy Diagnosed?
Bell’s palsy is essentially a diagnosis of exclusion. When other causes of facial palsy are removed, it is called isolated facial palsy Bell’s palsy or idiopathic facial palsy. Several other conditions can also cause facial paralysis, such as brain tumors, stroke, myasthenia gravis, and Lyme disease. If no specific cause can be identified, Bell’s palsy may be diagnosed.
Doctors can usually diagnose Bell’s palsy based on symptoms. There is no specific test to diagnose Bell’s palsy. However, your doctor may order tests to rule out other conditions that may cause similar symptoms and to determine the extent of nerve involvement or damage.
Bell’s Palsy Treatment
In the first couple of days to a week after the symptoms starts, a physiotherapist will evaluate the client and that includes a review of the medical history, when the symptoms began and what makes them worse or better and conduct a physical examination, focusing on identifying the patterns of weakness that are caused by Bell,s palsy such as:
Facial movements of the eyebrow
Eye closure
Ability to use the cheek in smiling
Ability to raise or lower the lips
Lip closure
Frowning
Facial expressions
Jaw and mouth movements
Forehead wrinkling
After the assessment, the physiotherapist will provide a customised Bell’s palsy treatment plan to help you regain the healthy pattern of movements that you need for facial expressions and function and coach throughout this challenging time, guiding you through special exercises that are designed to help you relearn facial movements based on your particular movement problems.
Eye care:
During the illness, most people with Bell’s palsy are unable to close their eyes on the affected side of the face. It is important to keep the eyes dry at night and while working at a computer. Eye care includes day time eye drops, a bed time ointment, or a night time moisturizing chamber to protect the cornea from scratches.
In the early stages of facial paralysis, the most important thing is proper care of the affected eye. Because the facial nerve is responsible for lubricating the cornea, you are very likely to suffer from dry eye during the first weeks and months of facial paralysis. This puts you at risk of developing corneal ulcers, which can impair your vision in the affected eye.
Your therapist will discuss dry eye treatment if it has not been done by another healthcare professional. If your eyes are red or red frequently, urgent referral to an ophthalmologist is needed. Alternatively, they should be advised to go to an ophthalmic emergency department.
Neuromuscular Retraining (NMR):
A paralyzed muscle contracts and shortens, causing a permanent contracture. A physical therapist can teach you how to stretch and strengthen your facial muscles to prevent this.
Neuromuscular retraining uses specific and precise feedback to enhance facial muscle activity in functional patterns of facial movements and expressions, and to inhibit aberrant muscle activity that impairs facial function. It’s a process of relearning.
In the early stages, if you have trouble generating or initiating movements, your physiotherapist will teach you exercises to initiate facial movements. Once you can start moving your facial muscles, your physical therapist will develop exercises to encourage muscle activity. This means increased muscle activity, stronger muscles, and improved ability to use muscles for longer periods of time.
Next, motor control exercises are introduced.
Improves facial muscle coordination. Correct any abnormal facial movement patterns that may occur during recovery.
Adjust facial movements for specific functions, such as speaking or closing your eyes.
Fine-tune facial expressions such as B. Smile.
Relaxation exercises are important during the recovery period as you may experience facial spasms and spasms. Physical therapists develop exercises to reduce this involuntary or unwanted contraction of specific muscles during other intended facial movements (sykinesis). For example, when you strain your neck muscles when you smile, or when you close your eyes and chew something.
A physical therapist teaches you how to recognize actual muscle contractions and when they are resting, guiding you to improve your ability to force facial muscles to contract and then stop. This relaxes the facial muscles and reduces spasms.
message therapy
Massage can help stretch and move facial muscles and improve blood circulation. This prevents complications such as contractures. Techniques such as using your fingertips to make circular motions around your cheeks can help increase the movement of your cheek muscles. These exercises can be done at home, but it is always recommended to seek professional help. It not only helps you combine techniques to effectively deal with problems, but it also helps you diagnose problems and prevent them from reoccurring .A Physiotherapist can help you get the best possible results incases of Bell’s palsy quickly and safely with proper facial exercises.
At Physiocare Physiotherapy, our trained therapists have experience with Bell’s palsy treatment. We can assess your case and guide you through your personalized rehabilitation process. Contact us today to book a complimentary consultation.

